Care for Burn Victims Better Adapted to Body Diversity

Purchased on Istockphoto.com. Copyright.
When a person with severe burns is admitted by hospital staff, assessing the extent of the injuries is urgent. Burns lead to significant fluid loss that must be replaced quickly to maintain homeostasis in the body. The quantity of fluid to be administered must be matched to the patient’s needs, based on the ratio of the burned skin area (%TBSA) to the total area (TBSA). Accurate assessment of this ratio is critical to providing optimal care. However, it is currently obtained by visual assessment, using 2D diagrams—which look like Leonardo da Vinci diagrams—not suited to different morphologies (Figure 1). The assessment is therefore highly dependent on the experience of the professional who is performing it. Current clinical methods result in over or underestimations of %TBSA of up to 161% [1, 2], which can cause serious complications and even death in more than 20% of cases [3]. Therefore, there must be a method adapted to body diversity that can personalize the patient’s morphology.
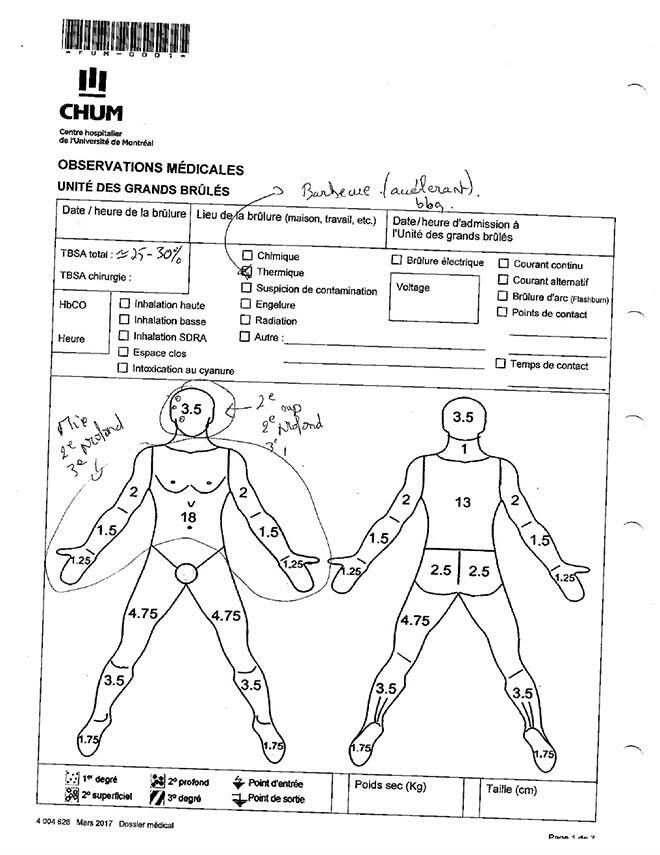
Figure 1: Lund and Browder chart used in the CHUM Burn Unit to assess the burned skin ratio. With permission.
Automatic Estimation of Patient’s Morphology
Optical methods now exist to access the 3D information of the anatomy of a human subject [4, 5, 6]. However, these methods are time consuming and require access to the entire subject, who must stand still for several minutes. This is not suitable in emergency situations or clinical settings in general [7].
An original 3D modeling method of the entire skin surface of a patient using a limited number of measurements and machine learning tools was developed in our laboratory (LIO, Imaging and Orthopaedics Research Laboratory) [7, 8, 9, 10]. To date, these measurements must be performed by the nursing staff using a tape measure, which can be difficult in emergency situations and when the patient cannot be moved—as is usually the case for patients with severe burns. A prototype mobile application has already been developed (Figure 2) to generate a 3D model of the body surface from the morphotype and from 3 to 4 anthropometric measurements—height, chest, neck and waist circumferences. The idea is to simplify and automate the measurement process to avoid any contact with the patient, while obtaining an accurate assessment of the total body surface area and the burned surface area.
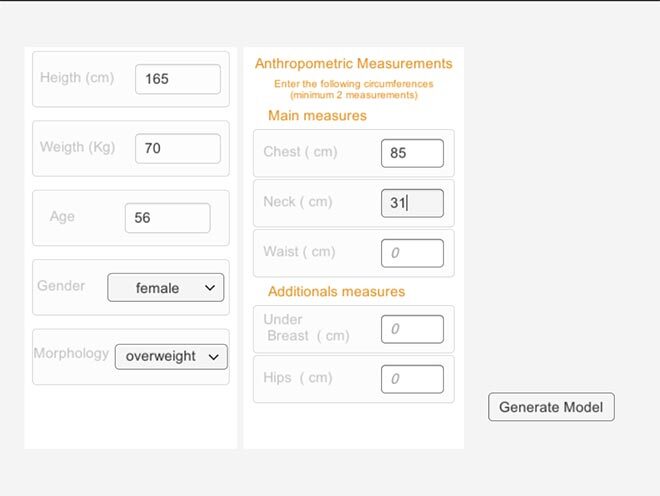
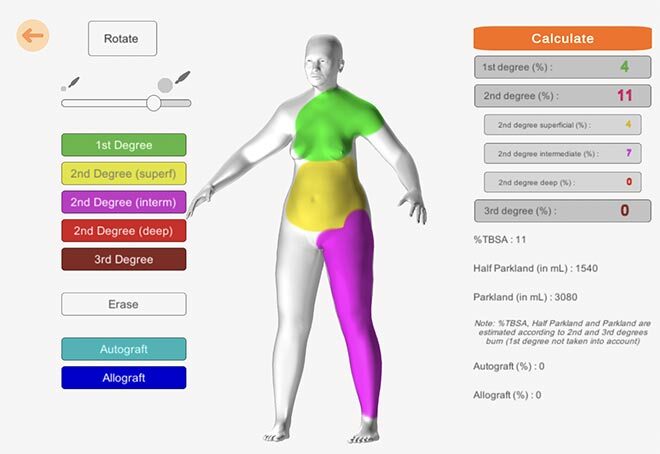
Figure 2: Image of the Mobile Application Prototype. Data entry page to produce a personalized 3D model of the patient (top). Burned area visualization and calculation page (bottom).
Burned Skin Surface Estimation Tool
The main goal of this research project is to propose a non-contact method based on the use of digital tools (e.g. smartphones, tablets) to estimate the burned surface area of patients in an emergency clinical setting. The objectives are:
- To develop an automated method of extracting anthropometric measurements from clinical data—patient photos, burns, 3D scans—to model the total body envelope of the patient.
- To develop an automated method of modeling and quantifying burned body surfaces from images of patient burns.
- To evaluate the accuracy and robustness of the developed methods.
To this end, data (e.g. photos of the patient, burns, 3D scans) will be acquired using digital tools including a camera and depth sensor. Anthropometric measurements will be extracted from the patient’s images and the 3D data using computer vision methods. They will allow the creation of a personalized 3D model of the patient using the method developed at the LIO (the Desbois Method).
The burned surfaces will then be segmented on the photos of the patient’s burns. An automatic registration of these images will be performed on the 3D model for each corresponding body part—using machine learning and texture mapping methods. Once the total and burned body surfaces have been estimated, these data will be used to calculate the %TBSA.
Finally, the developed methods will be evaluated with the participation of health professionals from the CHUM Burn Unit in order to validate their use in a real health care setting.
A Project of Great Significance for Patients
This research project was developed in a living laboratory context based on a clinical need identified and expressed by clinicians involved in the management of these patients. The goal of the project is to reduce the error rate in %TBSA estimation to:
- Optimize patient management with more personalized care.
- Reduce the risk of death and minimize long-term debilitating effects.
- Direct the patient to the appropriate facility—emergency room or specialty center—and limit the costs of unnecessary transfers.



