Abstract
We conducted a systematic mapping study (SMS) of works assessing the use of the HL7 FHIR standard to improve health information exchange at the semantic level.
We searched ten electronic databases as sources of information for inventory and review studies published during the period of 2012-2022 to investigate semantic interoperability efforts using the FHIR standard.
There is still no broad consensus in the healthcare community on how to achieve full semantic interoperability between information systems. Considerable efforts are being deployed to eliminate patient data silos and ensure semantic interoperability using the FHIR standard and terminologies.
This SMS outlines a categorization of FHIR-based approaches to semantic interoperability at different stages: extraction, annotation, modeling, mapping, transformation. This study argues that ML/NLP has recently emerged for unstructured data, and their use looks promising. Additionally, there is a need for tools to automate annotations and terminology services to accelerate the use and adoption of terminologies.
Keywords: EHR; HL7 FHIR, Interoperability; Data integration, Semantic; Terminology, SNOMED, LOINC, NLP
Introduction
The exponential growth of patient data acquisition sources, whether at home or in healthcare facilities (IoT healthcare devices, Electronic Health Record (EHR) systems) has resulted in data fragmentation, stored in multiple locations and in various formats (structured and unstructured). This brought several interoperability challenges across devices and systems [1], [2].
Interoperability in Healthcare: The Value of Standardization
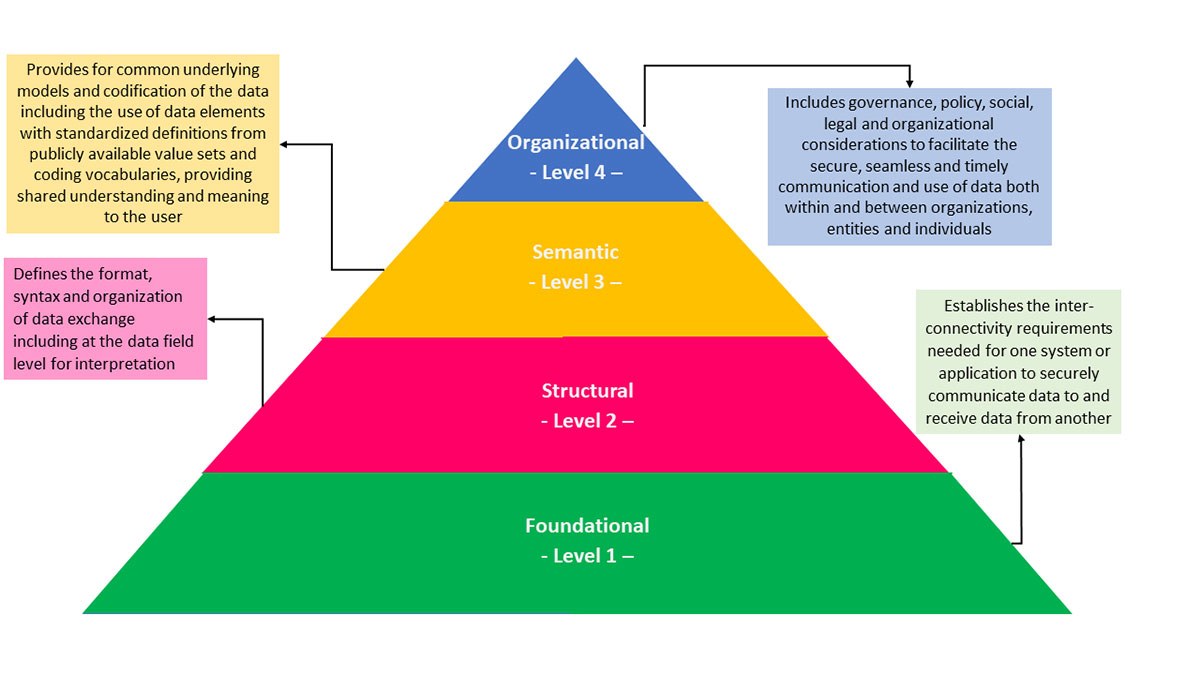
According to IEEE, Interoperability is defined as the “ability of two or more components to exchange information and to use the information that has been exchanged” [3]. A four-level framework was proposed by the Healthcare Information and Management Systems Society (HIMSS) [4]:1) foundational, 2) structural, 3) semantic, and 4) organizational (Figure 1).
The Fast Healthcare Interoperability Resources (FHIR) has recently emerged as the leading interoperability standard for the exchange of healthcare data. The FHIR standard was developed by Health Level Seven International (HL7) with the aim of evolving messaging standards to achieve semantic interoperability [5] [6]. Major technology players like Amazon, Google, IBM, Microsoft, Oracle and Salesforce offer ready-to-use cloud services to promote FHIR adoption [7].
Systematic Mapping Studies
Systematic mapping studies (SMS) seeks to classify the research outcome based on fundamental questions tied to a specific topic [8].
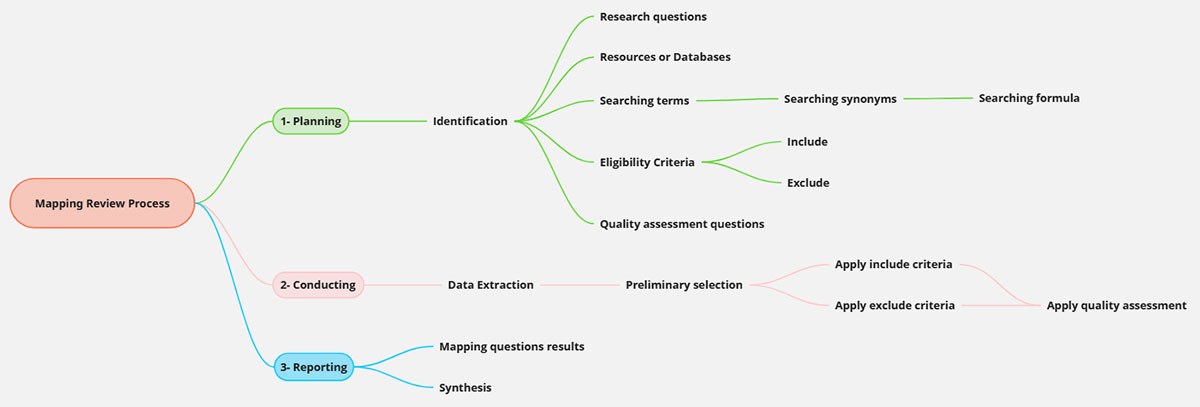
According to Perterson et al. [9], the mapping review process follows three steps: 1) planning, 2) conducting, and 3) reporting of mapping results. Moreover, Brereton et al. [10] provide guidance for the software engineering domain, outlining the tasks for each stage (figure 2):
- Planning: identification of all items required for the research process, including research questions, resources/databases, search terms and formulas, inclusion and exclusion criteria, and questions for quality assessment.
- Conducting: this stage includes the initial extraction of the studies as well as the pre-selection based on the inclusion and exclusion criteria. The selected studies were then evaluated and filtered using quality-assessment questions.
- Reporting: the selected studies are used for mapping and a discussion of the results is presented.
The goal of this SMS study was to present state of the art, trends and analysis of the research work related to semantic interoperability using FHIR. Specifically, this activity aimed to identify the FHIR resources and terminology used, as well as the different proposed approaches, contribution types and trends.
Ten databases served as primary data sources for this research: IEEE Xplore, Science Direct, Springer, Scopus, ACM, Web of Science, MedLine/PubMed, Compendex, Inspec, and Semantic Scholar.
Studies were considered if they were published between 2012 and 2022, in English or French. Additional criteria were applied to exclude duplicate studies, technical reports, 2 or 3 page book and study reports.
Assessing the quality of a research publication is a crucial selection step to ensure that the selected studies have the appropriate impact for mapping reviews and further analysis [8]. For this purpose, we defined quality criteria scores based on a list of questions. Quality evaluation of the identified/extracted studies was performed by answering each QA question. The selected studies met at least four of the six QA criteria. The others were rejected.
Semantic Interoperability Landscape
Data semantization involves different steps: data collection/extraction and annotation, modeling EHR data from legacy systems, and applying transformation and mapping to FHIR models and terminologies.
FHIR enables the use of international terminologies, including the following:
- SNOMED CT: multilingual clinical terminology standardized for EHR use. Its components include concepts (codes), descriptions (terms) and relationships.
- LOINC: A set of universal names and codes for the identification of laboratory and clinical test results.
We reviewed 70 selected studies and identified the most frequent data used for observation, medication and patient problem list. SNOMED-CT (32%) and LOINC (26%) were the most frequently used terminologies.
Six main semantic research approaches were identified from the solutions proposed in the 70 selected studies.
- Mapping to FHIR terminology (mapping) (25%);
- Transformation/development/validation of Resource Description Framework (RDF/OWL) (19%);
- Machine Learning/Natural Language Processing (ML/NLP) (16%);
- Semantic annotation (annotation) and terminology services (terminology) (14%); and
- ontology-based approach (ontology) (12%).
The selected studies used at least one of the six identified semantic research approaches, and most studies used more than one research approach.
The SMS highlights the fact that ML/NLP-based proposals emerged in 2018 in FHIR semantic interoperability studies, while the other approaches cover the full-time period.
In terms of type contribution within each of the 70 selected studies, five main contributions were identified.
- New framework or architecture to enable semantic interoperability (proposed framework/architecture) (37%);
- Evaluation or comparison of different techniques (e.g., ontology comparison) (15%);
- A new ontology model or enhancement of an existing one (model proposal) (19 %);
- A new technique or improvement of an existing technique (new technique proposal) (19 %); and
- A proposal based on the development of a new tool or on improving existing ones to facilitate semantic interoperability (tool proposal) (12%)
Conclusion
There is as yet no broad consensus in the healthcare community on how to achieve full semantic interoperability between information systems. The following key findings presented in this study provide researchers with an inventory of the approaches used to achieve semantic interoperability:
- Most studies were centred on clinical data resources; therefore, the focus has been on patient summary.
- Terminology mapping to SNOMED CT and LOINC was performed in more than half of the selected studies. None of the five approaches were dominant in the proposed solutions to the challenges of semantic interoperability.
- Most of the selected studies proposed a framework or architecture as a solution to enable semantic interoperability.
- Semantic interoperability remains an active area of research. Research on semantic interoperability has increased since 2018.
- The use of ML/NLP for unstructured data is promising and has been applied to specific use case scenarios.
- Terminology services are needed to accelerate their use and adoption.
- Effective techniques and tools are required to automate annotation and compare ontologies.
Additional Information
For more information on this research, please read the following research paper: Amar F, April A, Abran A
Electronic Health Record and Semantic Issues Using Fast Healthcare Interoperability Resources: Systematic Mapping Review. J Med Internet Res 2024;26:e45209. doi: 10.2196/45209



